Firefighters: Higher Risk of Venous Insufficiency and Vascular Disease
One might think that the biggest cause of injury among American firefighters would be burns and collapsing structures. However, more than just skin and bones, it is the firefighter’s vascular system that is at risk.
There are a number of reasons why firefighters are especially susceptible to vascular injury, and why they in particular need to consult with a qualified vein specialist for diagnosis and treatment of all dysfunctions that affect the heart and blood vessels, including Chronic Venous Insufficiency (CVI) and varicose veins.
Firefighters are Pushed to the Limit
The schedule of a firefighter is highly unpredictable. Shift work, itself, is disruptive to sleep and eating schedules, and can lead to generalized fatigue and difficult digestion. Unless an individual is motivated, the sometimes long periods of relative inactivity between fire calls can lead to weight gain and decreased levels of fitness; the incidence of overweight and obesity among firefighters is high. And adrenaline-drenched episodes of fire fighting push firefighters to the limit, physically, psychologically and emotionally. Working in the blistering heat, in heavy protective gear, hauling heavy equipment over long distances causes firefighters’ bodies to overheat and dehydrate, their blood vessels to dilate and become less efficient, and their blood more likely to coagulate easily.
Chronic Venous Insufficiency is Common among Firefighters
All of these are factors in the development of cardiovascular disease, including sudden cardiac events. Even more common among firefighters, though, is the development of Chronic Venous Insufficiency. While CVI is not likely to be fatal, it will adversely affect quality of life, and one’s ability to perform firefighting duties. Among other CVI symptoms, sufferers will note that their legs feel heavy, achy, itchy, and tired. Left untreated,Chronic Venous Insufficiency can progress, leading to swelling in the legs, feet and ankles, leg ulcers that don’t heal easily, and Deep Vein Thrombosis (DVT).
The good news is that there is help. If you are experiencing any of the symptoms of CVI, consider consulting a qualified vein specialist as soon as possible.
Using thorough examination techniques and duplex ultrasonography, a qualified vein specialist will be able to assess and recommend a treatment plan tailored to your needs. And there are minimally invasive techniques available that can help optimize your vascular health, with minimal discomfort, and in very little time have you back up and saving the world again, one burning building at a time.
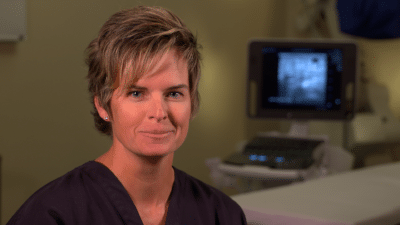
Entrevista con el Dr. Rose Durante nuestras entrevistas en video con Jilanne Rose le pedimos que nos contara algunas historias sobre sus experiencias en el tratamiento de las varices a lo largo de los años. Esta historia se trata de un paciente que se había despojado de las venas realizadas hace años y tenía miedo…
Read MoreDr. Rose Interview During our video interviews with Jilanne Rose we asked her to tell us some stories about her experiences in Varicose Veins Treatment over the years. This story is about a patient who had vein stripping performed years ago and was afraid of going through the process again because of the pain she…
Read MorePregunta: ¿puede usted conseguir congestión pélvica cuando usted nunca ha estado embarazado, y puede interferir con flujo de la orina?
Read MoreQuestion: Can you get pelvic congestion when you have never been pregnant, and can it interfere with urine flow? Answer: Pelvic congestion syndrome, although uncommon, can occur in women who have not been pregnant. These varicose veins in the lower abdomen typically do not cause problems with urination. Best to be evaluated by a gynecologist…
Read MorePregunta: tengo dolor y venas de araña apareciendo sobre todo en la zona del muslo después de mi ablación que fue hace 2 meses. GSV cerrado y SSV bien. Estoy usando 20-30 mmHG medias de rodilla-alta todos los días. ¿Cuál es la causa?
Read MorePregunta: tuve tratamiento de la escleroterapia de la espuma para la vena varicosa hace 2 meses por una técnica llamada catéter de flebogrif y leí que puede causar complicaciones como el movimiento. ¿Sigue siendo probable el riesgo? ¿Y qué sucede con la sustancia química usada en la espuma después de la inyección, permanece en el…
Read MoreQuestion: I had foam sclerotherapy treatment for varicose vein 2 months ago by a technique called flebogrif catheter and I read that it may cause complications like stroke. Is the risk still probable? And what happens to the chemical substance used on the foam after the injection, does it remain in the blood stream and…
Read MoreQuestion: I have pain and spider veins popping up mostly in the thigh area after my ablation which was 2 months ago. GSV closed and SSV ok. I am wearing 20-30 mmHG knee-high stockings every day. What is the cause?
Read MorePregunta: ¿Cuánto tiempo toma la cirugía de la vena varicosa en sí misma y cuánto hora debo esperar para la recuperación?
Read MorePregunta: ¿Qué puede decirme un examen de reflujo venoso? ¿Cómo mide el tratamiento la efectividad de mis venas?
Read More