Firefighters: Higher Risk of Venous Insufficiency and Vascular Disease
One might think that the biggest cause of injury among American firefighters would be burns and collapsing structures. However, more than just skin and bones, it is the firefighter’s vascular system that is at risk.
There are a number of reasons why firefighters are especially susceptible to vascular injury, and why they in particular need to consult with a qualified vein specialist for diagnosis and treatment of all dysfunctions that affect the heart and blood vessels, including Chronic Venous Insufficiency (CVI) and varicose veins.
Firefighters are Pushed to the Limit
The schedule of a firefighter is highly unpredictable. Shift work, itself, is disruptive to sleep and eating schedules, and can lead to generalized fatigue and difficult digestion. Unless an individual is motivated, the sometimes long periods of relative inactivity between fire calls can lead to weight gain and decreased levels of fitness; the incidence of overweight and obesity among firefighters is high. And adrenaline-drenched episodes of fire fighting push firefighters to the limit, physically, psychologically and emotionally. Working in the blistering heat, in heavy protective gear, hauling heavy equipment over long distances causes firefighters’ bodies to overheat and dehydrate, their blood vessels to dilate and become less efficient, and their blood more likely to coagulate easily.
Chronic Venous Insufficiency is Common among Firefighters
All of these are factors in the development of cardiovascular disease, including sudden cardiac events. Even more common among firefighters, though, is the development of Chronic Venous Insufficiency. While CVI is not likely to be fatal, it will adversely affect quality of life, and one’s ability to perform firefighting duties. Among other CVI symptoms, sufferers will note that their legs feel heavy, achy, itchy, and tired. Left untreated,Chronic Venous Insufficiency can progress, leading to swelling in the legs, feet and ankles, leg ulcers that don’t heal easily, and Deep Vein Thrombosis (DVT).
The good news is that there is help. If you are experiencing any of the symptoms of CVI, consider consulting a qualified vein specialist as soon as possible.
Using thorough examination techniques and duplex ultrasonography, a qualified vein specialist will be able to assess and recommend a treatment plan tailored to your needs. And there are minimally invasive techniques available that can help optimize your vascular health, with minimal discomfort, and in very little time have you back up and saving the world again, one burning building at a time.
Is there anything worse than itchy varicose veins? Maybe, but itchy veins remains high on the list of issues we would love to resolve before they drive us crazy. If you are experiencing itching around your varicose veins, it could be a message from your body that it is time to have your veins checked…
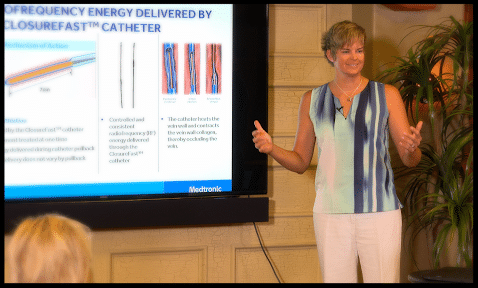
Read MoreThe full story on Chronic Venous Insufficiency, what it is and how to treat it. A video presentation by Jilanne Rose, DNP-C, Clinical Director. Run Time 24:46. TRANSCRIPT What’s the Difference Between Veins and Arteries? When we talk about vascular health and vascular disease most people think about arteries. When we talk about the…
Read MoreA group of Gilbert Arizona Residents concerned about Chronic Venous Insufficiency gathered on Saturday July 16th for an interactive discussion on CVI symptoms, causes and treatments. Chronic Venous Insufficiency, Venous Reflux Disease and Varicose Veins affect over 30 million American men and women. Unfortunately, many do not get treated as they believe varicose veins are…
Read MoreCan Chronic Venous Insufficiency (CVI) be reversed? Unfortunately the short answer to this question is no; but CVI can be treated with minimally invasive procedures which can reduce symptoms and improve quality of life tremendously! Chronic Vein Insufficiency Causes In order to understand why venous insufficiency or peripheral venous insufficiency cannot be reversed, we must…
Read MoreWhat can you do to treat bleeding varicose vein and spider veins? First and foremost, don’t panic. Although the visual effect of a ruptured varicose vein or bleeding vein can be alarming, there are some simple things that can be done to get the bleeding to stop. If you can reach the area that is…
Read MoreWhy are varicose veins painful? The discomfort associated with varicose veins is caused by a combination of factors. When veins are weak, the blood which is supposed to return to the heart in a timely fashion, settles and pools in the superficial vein system. This pooling of blood worsens when patients stand or sit in…
Read MoreEndovenous Ablation Definition Taken literally, endovenous ablation is the removal of a vein from within. ‘Endo’ means internal or inside, ‘venous’ refers to a vein, and ablation is to ‘remove’. In the instance of veins, it is no longer necessary to physically remove a vein from the leg (vein stripping) to improve symptoms or the…
Read MoreThe newest procedure for the treatment of varicose veins was approved by the FDA about two years ago. It is what has been termed a non-tumescent non-thermal therapy. What this means is that it does not require a lot of numbing medicine to complete, and it does not use a heating element to close or…
Read MoreWhat is the best treatment for varicose veins? No varicose vein is the same; no person’s symptoms are the same; and so the best procedure for varicose veins is not always the same. The treatments associated with vein disease are based on a patient’s symptoms, vein size, location, contributing conditions, and ultrasound findings. Different…
Read More