Care for Nurses with Chronic Venous Insufficiency

It can hurt to care--just ask any nurse.
As a profession, nurses experience some of the highest rates of varicose veins and Chronic Venous Insufficiency (CVI) in the country. In fact, in one study by the NIH, 63 per cent of participating nurses were shown to have at least one sign of CVI.
Nurses will know that it is important to diligently practice self-care in order to minimize the discomfort of this condition. Elevating the legs, compression stockings, and engaging in calf muscle-contracting exercises such as walking are just some of the home care remedies that can provide occasional relief. As a chronic and progressive condition, the pain, fatigue and other symptoms caused by CVI are likely to worsen.
Fortunately, there are other minimally invasive treatment options that can bring relief from the pain of CVI and varicose veins. If you live and work with any of these symptoms , consider consulting a qualified vein specialist soon to ensure your vascular health is not at risk, and to learn about a treatment plan that is tailored for you.
In the meantime, compression stockings helps if you stand or sit for long periods of time. However, be careful with calf sleeves as they can sometimes cause swelling in the feet because they typically end at the ankle.
CVI risk factors for nurses
There are a number of reasons why nurses are at particular risk for development and progression of CVI. The first reason is their job requires that they stand for long periods; basically, gravity takes its toll. Activities that require standing (or even sitting) for extended periods deprive the body of the benefits of the strong calf muscle contractions produced while walking. This means the heart has to work a lot harder to push the blood through the legs and back up for reoxygenation and recirculation. Over time, the vascular system wearies and becomes less efficient.
The physical strain of the occupation is another notable contributor to the development of CVI. Nurses work long hours, carry out very physical labor, and often perform shift work. This can affect sleep and eating schedules, and these factors can have a negative effect on health, generally, leading to conditions such as insomnia and overweight.
Another factor is gender. Women dominate nursing, and estrogen, oral contraceptives and hormone replacements are known to contribute to the weakening of blood vessel walls. This stretch in blood vessels means more bulging and less efficient return of blood.
Help for nurses with CVI
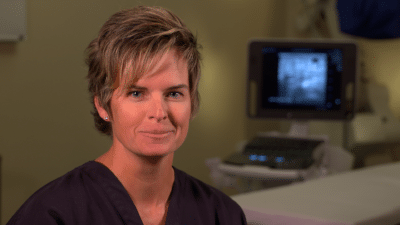
The good news is that there are qualified vein specialists who care about the wellbeing of nurses. Jilanne Rose is one such specialist. As a board certified doctorate nurse practitioner, she understands the special needs of nurses. Trained by three top Arizona vein specialists-an interventional cardiologist, a cardiothoracic surgeon, and an interventional radiologist-she has completed over 10,000 peripheral vein procedures, and is known for her compassionate care and exceptional outcomes.
If you are experiencing any of the symptoms of CVI, consider consulting with Jilanne today to find out how she can have you back on your feet and doing the work you love, more comfortably, in remarkably little time.
Entrevista con el Dr. Rose Durante nuestras entrevistas en video con Jilanne Rose le pedimos que nos contara algunas historias sobre sus experiencias en el tratamiento de las varices a lo largo de los años. Esta historia se trata de un paciente que se había despojado de las venas realizadas hace años y tenía miedo…
Read MoreDr. Rose Interview During our video interviews with Jilanne Rose we asked her to tell us some stories about her experiences in Varicose Veins Treatment over the years. This story is about a patient who had vein stripping performed years ago and was afraid of going through the process again because of the pain she…
Read MorePregunta: ¿puede usted conseguir congestión pélvica cuando usted nunca ha estado embarazado, y puede interferir con flujo de la orina?
Read MoreQuestion: Can you get pelvic congestion when you have never been pregnant, and can it interfere with urine flow? Answer: Pelvic congestion syndrome, although uncommon, can occur in women who have not been pregnant. These varicose veins in the lower abdomen typically do not cause problems with urination. Best to be evaluated by a gynecologist…
Read MorePregunta: tengo dolor y venas de araña apareciendo sobre todo en la zona del muslo después de mi ablación que fue hace 2 meses. GSV cerrado y SSV bien. Estoy usando 20-30 mmHG medias de rodilla-alta todos los días. ¿Cuál es la causa?
Read MorePregunta: tuve tratamiento de la escleroterapia de la espuma para la vena varicosa hace 2 meses por una técnica llamada catéter de flebogrif y leí que puede causar complicaciones como el movimiento. ¿Sigue siendo probable el riesgo? ¿Y qué sucede con la sustancia química usada en la espuma después de la inyección, permanece en el…
Read MoreQuestion: I had foam sclerotherapy treatment for varicose vein 2 months ago by a technique called flebogrif catheter and I read that it may cause complications like stroke. Is the risk still probable? And what happens to the chemical substance used on the foam after the injection, does it remain in the blood stream and…
Read MoreQuestion: I have pain and spider veins popping up mostly in the thigh area after my ablation which was 2 months ago. GSV closed and SSV ok. I am wearing 20-30 mmHG knee-high stockings every day. What is the cause?
Read MorePregunta: ¿Cuánto tiempo toma la cirugía de la vena varicosa en sí misma y cuánto hora debo esperar para la recuperación?
Read MorePregunta: ¿Qué puede decirme un examen de reflujo venoso? ¿Cómo mide el tratamiento la efectividad de mis venas?
Read More