Care for Nurses with Chronic Venous Insufficiency

It can hurt to care--just ask any nurse.
As a profession, nurses experience some of the highest rates of varicose veins and Chronic Venous Insufficiency (CVI) in the country. In fact, in one study by the NIH, 63 per cent of participating nurses were shown to have at least one sign of CVI.
Nurses will know that it is important to diligently practice self-care in order to minimize the discomfort of this condition. Elevating the legs, compression stockings, and engaging in calf muscle-contracting exercises such as walking are just some of the home care remedies that can provide occasional relief. As a chronic and progressive condition, the pain, fatigue and other symptoms caused by CVI are likely to worsen.
Fortunately, there are other minimally invasive treatment options that can bring relief from the pain of CVI and varicose veins. If you live and work with any of these symptoms , consider consulting a qualified vein specialist soon to ensure your vascular health is not at risk, and to learn about a treatment plan that is tailored for you.
In the meantime, compression stockings helps if you stand or sit for long periods of time. However, be careful with calf sleeves as they can sometimes cause swelling in the feet because they typically end at the ankle.
CVI risk factors for nurses
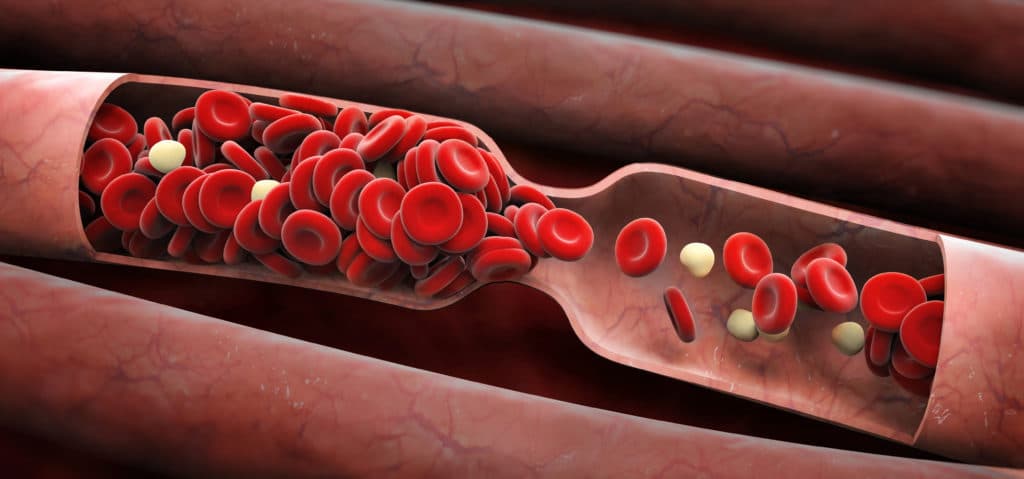
There are a number of reasons why nurses are at particular risk for development and progression of CVI. The first reason is their job requires that they stand for long periods; basically, gravity takes its toll. Activities that require standing (or even sitting) for extended periods deprive the body of the benefits of the strong calf muscle contractions produced while walking. This means the heart has to work a lot harder to push the blood through the legs and back up for reoxygenation and recirculation. Over time, the vascular system wearies and becomes less efficient.
The physical strain of the occupation is another notable contributor to the development of CVI. Nurses work long hours, carry out very physical labor, and often perform shift work. This can affect sleep and eating schedules, and these factors can have a negative effect on health, generally, leading to conditions such as insomnia and overweight.
Another factor is gender. Women dominate nursing, and estrogen, oral contraceptives and hormone replacements are known to contribute to the weakening of blood vessel walls. This stretch in blood vessels means more bulging and less efficient return of blood.
Help for nurses with CVI
The good news is that there are qualified vein specialists who care about the wellbeing of nurses. Jilanne Rose is one such specialist. As a board certified doctorate nurse practitioner, she understands the special needs of nurses. Trained by three top Arizona vein specialists-an interventional cardiologist, a cardiothoracic surgeon, and an interventional radiologist-she has completed over 10,000 peripheral vein procedures, and is known for her compassionate care and exceptional outcomes.
If you are experiencing any of the symptoms of CVI, consider consulting with Jilanne today to find out how she can have you back on your feet and doing the work you love, more comfortably, in remarkably little time.
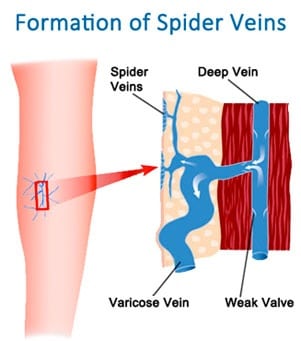
Question: I have spider veins on my legs and they really hurt to the touch. Can that be dangerous to my health? Answer: In the large picture, pain associated with spider veins is not life threatening. It would be worthwhile to have an evaluation by a qualified provider to see if these spider veins are…
Read MoreI am scheduled for a right leg radiofrequency ablation. I have venous insufficiency in the saphenous vein and have had a blood clot before. Question: In 2006, I underwent an artificial lumbar disk implant. This failed causing artificial disk to move into the spine. While surgeon removed the artificial disk implant, he nicked the liac…
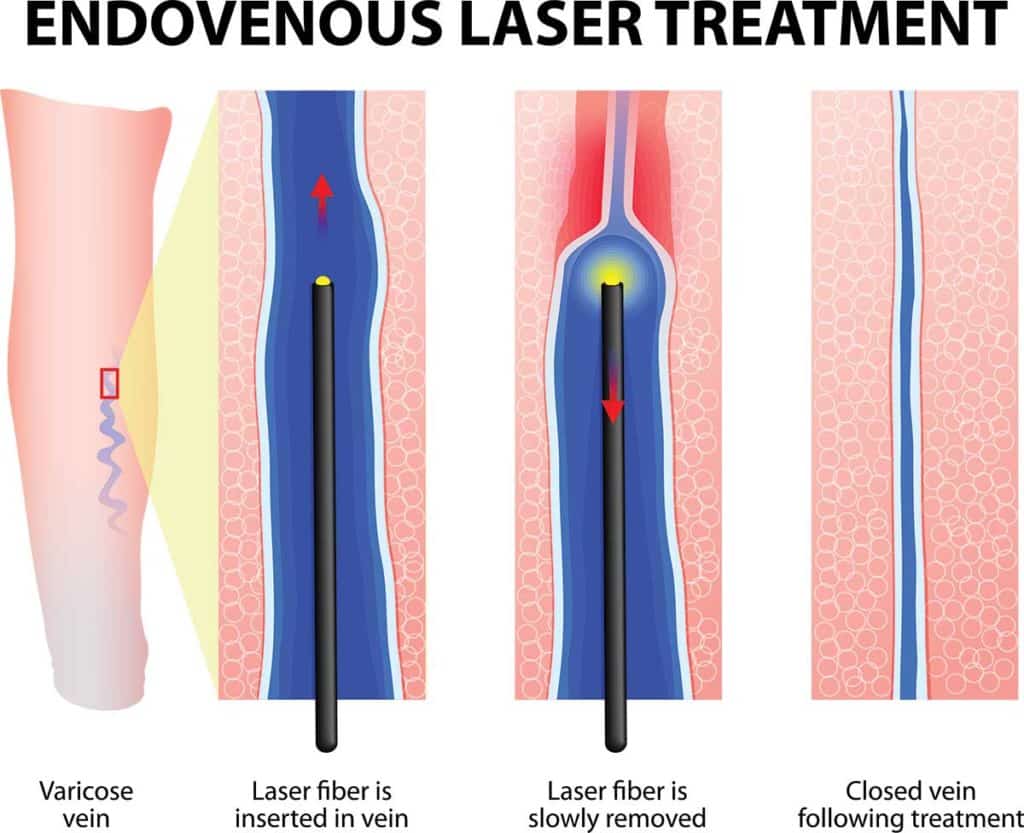
Read MoreMy doctor said my vein is too large to have sclerotherapy performed first, is this true? Question: I have a few visible spider veins on my lower leg that I want treated with foam sclerotherapy. However, the doctor wants me to do endovenous laser treatment before the sclerotherapy. According to him, my vein is way…
Read MoreI’m having the same pain that I had before my ablation procedure, except it is in a different new location. How long will this go on? Question: It’s been 2 months since my GSV endovenous laser ablation procedure. I have the same pain that I had before the procedure, except it’s in a new location.…
Read MoreI recently had the VNUS procedure done (both legs, multiple veins). Is it normal to have open, circular wound with redness and slight weepiness? Question: All of the other areas are healing nicely, but the area on my shin (a bit off center) has a much larger wound. It has been quite red in the…
Read MoreQuestion: How big of a size do compression stockings come in? Answer: Compression socks should be comfortable and supportive. If the stockings are making your symptoms worse, it is likely that they do not fit you correctly. There are numerous companies that make standard sized compression stockings. Some make 7 to 8 different sizes. Additionally,…
Read MoreQuestion: WHAT CAN I DO TO GET RID OF MY VARICOSE VEINS? Answer: There are numerous options to treat varicose veins. Some are considered medically necessary, while others are strictly cosmetic. Larger veins are treated in a myriad of ways depending on the provider you consult with and their proficiency in a given intervention. The…
Read MoreQuestion: I knelt down the other day and injured the large varicose vein over my knee. It bruised quickly and felt very sore, so I put a pressure bandage on it. Since then, the vein bruise has spread and is now about 12″ up my thigh. It is very red, and I’m not sure what…
Read MoreQuestion: What treatment options are available for my CVI? I can’t sit or stand in one place and I have heavy, aching legs all of the time. I started to have achy, heavy leg feelings about a month after I sprained my right ankle and scratched my left knee last April. I was diagnosed with…
Read MoreQuestion: During the EVLT laser procedure I really didn’t feel well, especially when the laser was on. I felt dizzy and the smell of “burning” freaked me out. Even after I was done, it took me couple hours to feel normal again. Is that normal? Answer: The “odor” and sometimes a taste is normal during…
Read More